Is It Flu, COVID-19, Allergies, or a Cold?
Staying Healthy This Winter
Feeling sick can be especially concerning these days. Could your sniffles be caused by COVID-19? Or the flu? A cold? Or maybe allergies?
Determining the cause of an illness can be tricky because many share some symptoms. They can leave you sniffling, coughing, and feeling tired. But there are important differences.
Figuring out what’s making you sick can help you recover and prevent spreading sickness to others.
Flu vs COVID-19
“Distinguishing COVID from flu can be difficult because the symptoms overlap so much,” explains Dr. Brooke Bozick, an NIH expert on respiratory diseases that affect the lungs.
Flu and COVID-19 are caused by different viruses that can be spread among people. Flu is caused by the influenza virus. COVID-19 is caused by SARS-CoV-2. Both can give you a fever, cough, headaches, and body aches.
Flu and COVID-19 also spread similarly. They’re transmitted by small particles that come from your nose and mouth when you sneeze, cough, sing, or talk, raising the possibility of infecting people who are nearby. Infected people may not have symptoms, but can still pass along either virus.
“Both influenza and COVID can be spread to other people before individuals develop symptoms,” notes Dr. Aubree Gordon, an infectious disease expert at the University of Michigan.
COVID-19 symptoms can take longer than flu symptoms to develop, she explains. Someone with flu usually has symptoms 1 to 4 days after being infected. A person with COVID-19 typically shows symptoms about 5 days after infection, although this can range from 2 to 14 days.
One telling sign of COVID-19 in some cases is loss of smell or taste. But because of other similar symptoms, there’s really only one way to be certain if you have COVID-19 or flu: Get tested.
“You can go and get a COVID test at many pharmacies, and your doctor can administer tests for flu,” Bozick says. COVID-19 tests are also available at many health centers. And you can buy testing kits approved for use at home.
Could It Be a Cold? Or Allergies?
Like flu and COVID-19, colds are also caused by viruses and can be passed to others.
Symptoms of a cold tend to be mild. You may have a runny nose, cough, congestion, and sore throat. But you won’t usually have the aches and fever that are common with COVID-19 and flu. Often, you’ll feel better in a couple of days.
There’s no cure for the common cold. Typical treatments include rest, fluids, and over-the-counter medicines. Some complementary treatments may help with cold symptoms, too. Taking honey may help with nighttime cough for children over 1 year old. Rinsing your nose and sinuses can help with congestion. You can use a neti pot or other nasal rinsing device. Be sure to only use water that’s been properly processed, such as distilled or boiled water, not tap water. Nasal rinses can bring relief for both cold and allergies.
Allergies can cause a runny nose and sneezing. But they’re not contagious. If your eyes, nose, or ears itch, that also could be an allergy.
Exposure to things like dust, pets, and tree or grass pollen can trigger allergies, which are caused by the The system that protects your body from invading viruses, bacteria, and other microscopic threats. immune system overreacting.
Allergy symptoms tend to stop when you’re no longer exposed to the cause. Unless you have asthma, allergies typically do not cause breathing problems. Allergies can be treated with drugs like antihistamines, decongestants, and nasal steroids.
Wintery Mix of Viruses
Winter is the prime cold and flu season. You’re more likely to be indoors and closer to others when it’s colder outside. Weather also plays a role in the spread of viruses.
“Cold and flu viruses survive better and are more transmissible if it’s cooler and if there’s lower humidity,” Gordon explains.
Experts are concerned that flu and COVID-19 cases may increase and overlap in the winter. Flu cases usually start to increase around October and peak between December and February. Being infected with flu and SARS-CoV-2 at the same time is possible, as is showing symptoms of both.
If you’re sick with the flu, your doctor may prescribe antiviral drugs. Such drugs can make your flu milder and shorten the time you are sick. They work best if they’re used early in your illness.
The FDA has also approved one antiviral drug, called remdesivir, to treat COVID-19. Other treatments are in development and under review. No complementary approaches have been shown to be helpful for fighting off flu or COVID-19.
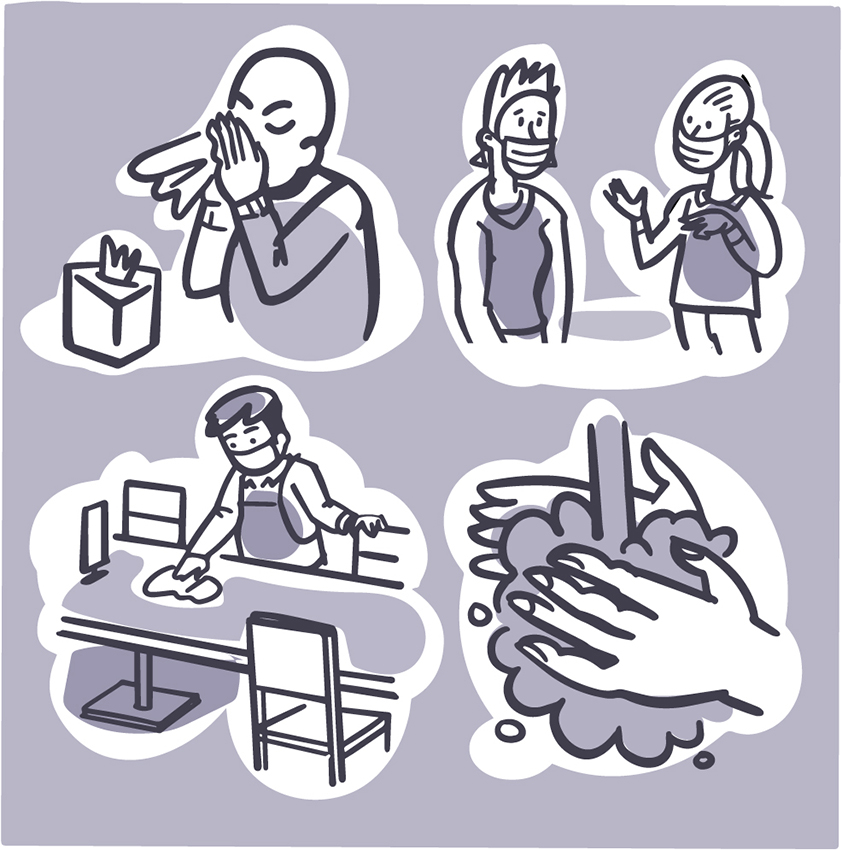
Fortunately, strategies to prevent the spread of COVID-19 also prevent the spread of flu and cold. “Measures like masking and social distancing work for other respiratory viruses, as well as COVID-19,” says Dr. Chip Walter, who studies vaccine development at Duke University.
Staying Well
There’s another really important way to fight viruses. “Get your flu shot and COVID-19 vaccine,” Walter advises. They are safe and effective ways to protect yourself and those around you.
Don’t forget to vaccinate your children, too. That is the best way to protect their health. COVID-19 vaccines are now recommended for everyone age 5 years and older.
Flu vaccines are recommended for everyone 6 months and older. Flu vaccines are designed to protect against the four types of flu viruses that scientists expect to circulate that year.
Researchers like Walter and others are working to develop flu vaccines that last longer and offer broader protection against many flu strains.
Masks continue to be an important tool for stopping the spread of respiratory viruses, such as COVID-19. “With the pandemic still ongoing, it’s going to be really important that people wear masks,” Gordon says. Try to avoid crowded indoor situations when possible, too.
For more tips on guarding against getting sick this winter, see the Wise Choices box.
Comparing Cold, Flu, Allergies, and COVID-19 |
||||
|---|---|---|---|---|
| Symptoms | Cold | Flu | Airborne Allergy | COVID-19 |
| Fever | Rare | Usual, high (100–102 °F), sometimes higher, especially in young children); lasts 3–4 days | Never | Common |
| Headache | Uncommon | Common | Uncommon | Common |
| General Aches, Pains | Slight | Usual; often severe | Never | Common |
| Fatigue, Weakness | Sometimes | Usual, can last up to 3 weeks | Sometimes | Common |
| Extreme Exhaustion | Never | Usual, at the beginning of the illness | Never | Common |
| Stuffy, Runny Nose | Common | Sometimes | Common | Common |
| Sneezing | Usual | Sometimes | Usual | Rarely |
| Sore Throat | Common | Sometimes | Sometimes | Common |
| Cough | Common | Common, can become severe | Sometimes | Common, dry cough |
| Chest Discomfort | Mild to moderate | Common | Rare, except for those with allergic asthma | Common; can cause trouble breathing or persistent pain or pressure in the chest that calls for immediate emergency care |
| Loss of Taste or Smell | Rarely | Rarely | Rarely | Common |
| Treatment | Get plenty of rest. Stay hydrated. (Drink plenty of fluids.) Decongestants. Aspirin (ages 18 and up), acetaminophen, or ibuprofen for aches and pains |
Get plenty of rest. Stay hydrated. Aspirin (ages 18 and up), acetaminophen, or ibuprofen for aches, pains, and fever Antiviral medicines (see your doctor) |
Avoid allergens (things that you’re allergic to) Antihistamines Nasal steroids Decongestants |
NIH has developed guidance on treatment of COVID-19, which is regularly updated. The FDA has approved one drug, remdesivir, to treat COVID-19.* |
| Prevention | Wash your hands often. Avoid close contact with anyone who has a cold. |
Get the flu vaccine each year. Wash your hands often. Avoid close contact with anyone who has the flu. |
Avoid allergens, such as pollen, house dust mites, mold, pet dander, cockroaches. | Get the COVID-19 vaccine, recommended for everyone age 5 and older. Wear a mask in indoor public places. Avoid crowds. Wash your hands often and avoid touching your eyes, nose, and mouth. Get tested if you think you might have COVID-19. |
| Complications | Sinus infection middle ear infection, asthma | Bronchitis, pneumonia; can be life-threatening | Sinus infection, middle ear infection, asthma | Pneumonia, respiratory failure, acute respiratory distress syndrome (fluid in lungs), sepsis, cardiac events (e.g., heart attack and stroke), multiple organ failure, inflammation of the heart, brain, or muscle tissue, death |
*Editor’s Note: Treatment guidelines are evolving. Remdesivir was the only drug approved at the time this article was written. Talk with your doctor about currently available medications.
NIH Office of Communications and Public Liaison
Building 31, Room 5B52
Bethesda, MD 20892-2094
nihnewsinhealth@od.nih.gov
Tel: 301-451-8224
Editor:
Harrison Wein, Ph.D.
Managing Editor:
Tianna Hicklin, Ph.D.
Illustrator:
Alan Defibaugh
Attention Editors: Reprint our articles and illustrations in your own publication. Our material is not copyrighted. Please acknowledge NIH News in Health as the source and send us a copy.
For more consumer health news and information, visit health.nih.gov.
For wellness toolkits, visit www.nih.gov/wellnesstoolkits.




